Implanting a pacemaker
Before the procedure
Before the procedure, you will need to blood tests, e.g. to check for infections and cell counts. If you have any bleeding disorder or if you are on blood-thinning medications, please let your doctor know; you may be asked to pause some of these medications before the procedure. If you have any allergies or in case you are/ may be pregnant, you should inform your doctor.
The day before the procedure, you may be asked to wash your whole body with a special soap. You will also be requested to fast for some time, usually overnight, as sedatives or general anesthesia might be required during the procedure which can only be given safely when your stomach is empty. This includes any food or drink (inclusive water, chewing gums or smoking). If you should take some medications in the morning before the procedure, you should take them with a small sip of water.
Other specific preparation can sometimes be necessary, depending on your general medical condition.
During the procedure

The procedure of implantation may vary depending on your condition and the type of device you need. Such a procedure can be performed in an outpatient setting or during a short hospital stay. A pacemaker implantation usually takes 1-2 hours, but the Implanted Cardiac Device (ICD) or CRT (Cardiac Resynchronisation Therapy) implantation can take more time. The hospital stay needed can vary depending on the type of the device implanted and the local routines.
During the procedure you will need to lay on your back for some time. If you suffer of a condition that makes that difficult (e.g. severe back pain), you should notify your doctor.
The procedure is usually performed with local anesthesia, which means that you will remain awake, but you will probably receive sedative drugs to help you relax. You will also need to receive antibiotics to prevent an infection after the procedure. To administrate fluids and medications during the procedure, if needed, an intravenous line will be placed in a vein in your arm or hand.
As soon as you are placed on the operation table, you will be connected to an ECG monitor using electrodes to monitor your heart rhythm during the procedure. Your blood pressure, breathing rate and oxygen level will also be monitored during the procedure by a nurse. The incision site in the chest will be cleaned with a specific soap and any excessive hair may be clipped. Sterile sheets will be placed around this area to keep it sterile.
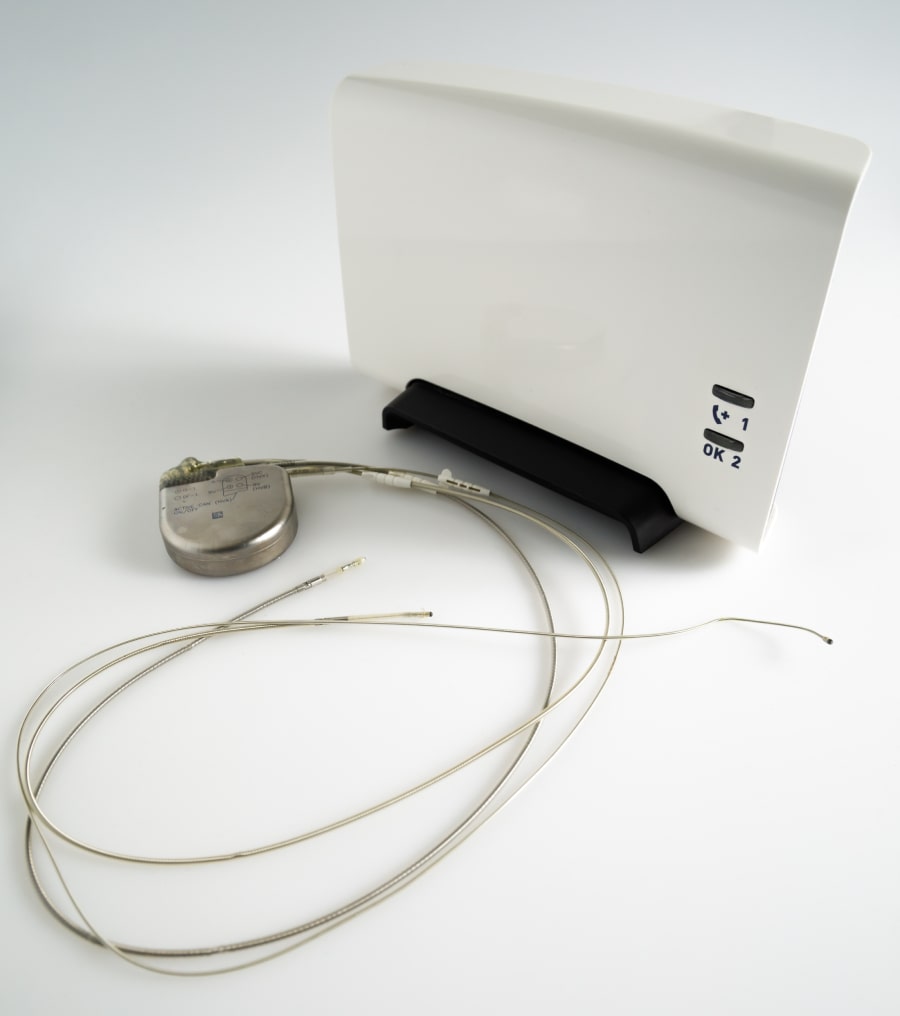
In most cases, general anaesthesia will not be needed since the incision is small. Local anesthesia will be injected at the selected site to numb the area usually providing sufficient pain control. If you are very anxious, please discuss with your physician, it is often possible to administer medication that helps to relax. The doctor will then proceed with the incision at the site under the collarbone where the generator will be placed later. Small plastic tubes, called sheaths or introducers, will be inserted into a vein that passes under the collarbone. One or more leads (insulated wires) will be placed through the introducers into the vein and will be guided into the heart using X-ray images. Once the leads are inside the proper chamber of the heart (depending on the type of the device and the chamber which will be treated), some tests will be done to confirm the location and to check they work well. The leads will then be secured. The other end of the leads will be connected to the pulse generator and the generator will be placed under the skin at the site of the incision. Usually, the generator is placed in the upper left chest. The incision will be closed with sutures or surgical glue and a sterile bandage will be applied.
If a leadless pacemaker is being implanted, the procedure required is less invasive. The insertion site is through the femoral vein at the top of the leg, where, after injecting local anesthesia to numb the area, a flexible sheath will be inserted in the vein and guided in the heart and into the right ventricle. A tiny leadless pacemaker (which contains both the generator and the other parts of the pacemaker), Is passed through the sheath and guided into the appropriate place in the right ventricle, where tests will be done to confirm it is in a good position. Then, the sheath will be removed from the body and the incision site will be closed, by applying pressure and often a temporary suture.
After the procedure

After the procedure, you will be taken to your hospital room or at the recovery room for observation for a few hours. Your heart rhythm and blood pressure will be monitored by a nurse. If you feel chest pain, dizziness or other discomfort, you should notify the nurse immediately. After a few hours, you may get of your bed carefully, with the assistance of the nurse. Once the observation time is completed and you recover, you may eat and drink.
You may be discharged from the hospital at the same day or the day after. Your device may be checked before discharge to make sure it works properly. If you are discharged the same day, you should have someone to accompany you home, due to the sedative drugs taken during the procedure. Before discharge, ask for instructions on how to manage your device, as well as advice on follow-up appointments, exercise, driving, medication, care and resumption of normal activities.
The incision site is usually a few centimeters long. It can be swollen and painful the first days after the procedure and painkillers may be needed. You will also experience itching skin around the wound for some time after surgery, which is quite normal. The incision should be kept dry and clean (your nurse should give you more instructions before discharge). Before discharge from the hospital, you will be given instructions how to treat the incision to reduce the chance of an infection and allow proper healing. Everyone heals differently but, in most patients, the scar fades away after the healing period and is not much perceptible. Depending on a person’s stature, the type of device (ICD being bigger than pacemakers) and how it was implanted, a small bulge may be visible on the implant site. Nevertheless, it should not be visible under clothes. If you are concerned about the cosmetic outcome of the procedure, please do speak with your physician before the implant.
Your doctor (or nurse) will check your device a some weeks or months after surgery to make sure the device works properly and there are no signs of complications. Nevertheless, you should contact your doctor in case you experience any of the following after device implantation.
- Symptoms or complaints you also felt before device implantation.
- Blackouts/fainting spells.
- Increased shortness of breath, chest pain or dizziness.
- Direct contact is necessary when there is a suspicion of an infection, for example in case of fever (>38,5gr C), chills or sweats, redness or swelling of the device pocket, leaking or progressive pain from the incision site.
- Bleeding from the incision site or if the incision edges begin to pull apart.
- In case of an alert, some devices than can either beep or vibrate. Ask your physician or nurse if your device has this capability; if it does, they can give you a demonstration of the sound/vibration, so you are better prepared.
If not stated otherwise by your doctor, you should be able to return to your job and daily activities within a couple of weeks. You do not need to restrict arm movements and/or use an arm sling after device implantation, as this has not been shown to reduce risk of lead dislodgment and may increase shoulder pain. Before resuming your exercises/sports, it is best to consult your doctor for advice. If your stitches need to be removed, your doctor will inform you when and where to do it. Regarding driving, you should ask your doctor for instructions.
Routine follow-ups

Once you have a cardiac device, you will need to have regularly follow-ups by a doctor, or a nurse specialized on device programming.
The first follow-up is usually scheduled 2-12 weeks after the implantation of the device. The doctor or technician will inspect the incision site to check if it has healed properly without any signs of infection. Then they will perform a technical check, using a specific computer (programmer) which will connect to your device.

During the technical check, the doctor or technician will make several tests to confirm the appropriate function of the leads. You may briefly feel your heart rhythm go faster or slower than normal, which can cause some discomfort for a few seconds. This is totally normal and will disappear as soon as the test is finished. The doctor or technician may change some settings of your device during the follow-up to make the device more effective.
After the first follow-up, you will be scheduled to regular follow-ups once per year or so or rarely more often if needed.
Remote monitoring of cardiac devices has been developed for technical check-ups using transtelephonic data transmission. In addition, automatic or patient-triggered alerts can be sent to you cardiologist or technician. Remote monitoring can also be used to replace routine hospital visits for checkup on the programmable settings, device function, arrhythmias, cardiovascular hemodynamic function and registration of stored arrhythmias.
It should be noted that the remote monitoring transmitter has to be in close proximity of you to be able to communicate with the device. When the transmitter has received the data from the cardiac device it sends its data encrypted to the central server of the manufacturer of the device so it becomes accessible for the cardiologist or technician to evaluate. Remote monitoring cannot reprogram the device (to avoid any potential threat for the patient). Check with your hospital or cardiologist to see how remote monitoring is used in your area.
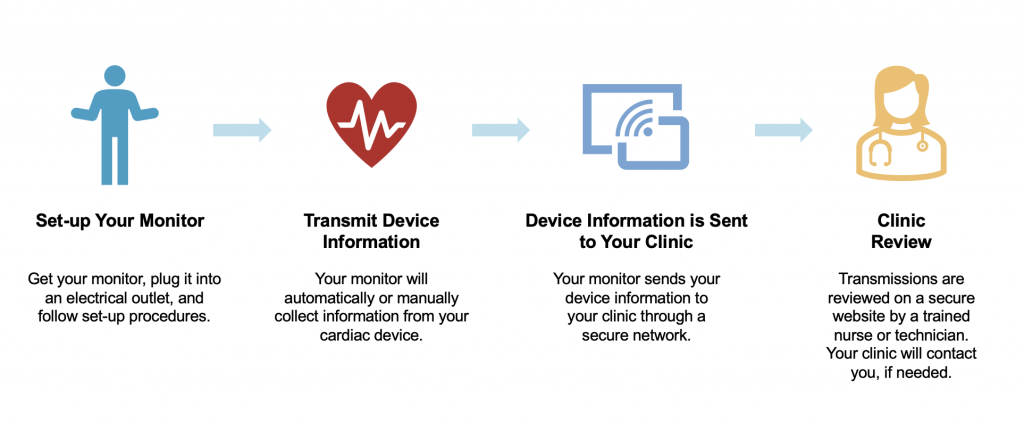
Currently, remote monitoring is expanding rapidly across Europe but the methodology and practicality varies considerably between countries and hospitals.
What does my device ID tell me/how to read my device ID?
The device identification card contains your personal information, contact details of your hospital and key information about your cardiac device. Therefore, it is important you always carry this ID card with you. The specific cardiac device details on the card include the manufacturer of the device, whether it is a pacemaker or ICD, the model and serial number, the type and manufacturer of the leads and date of device implantation.
Generator change
When the battery of the device reaches the end of its life (usually after 7-10 years, but sometimes less), the generator needs to be changed. If the leads are intact and work perfectly, there is no need to replace them. The battery of the device will not end suddenly and unexpectedly. From the time it reaches what is called elective replacement indicators, it usually has at least 3 months of extra battery lifetime. This means that there is plenty of time to plan for a change.
The preparation for the replacement of the generator is similar with the preparation for a device implantation (see above). The procedure, however, is much simpler with fewer complications if no leads need to be added or replaced. An incision will be made at the implantation site of your device. The old generator will be disconnected from the leads and will be replaced by the new one in the same place. The new generator will then be connected to the electrodes. The device will be programmed and then the incision will be closed with sutures.
The observation time after the procedure is usually short and you will be probably discharged the same day.
What are the risks and Complications

A pacemaker or ICD implantation is a routine procedure in most hospitals; thus, complications are infrequent. The most important complications are summarized below:
- Pneumothorax/ hemothorax: This is a condition where the lungs can accidentally be damaged during the procedure, resulting in air (pneumothorax) or blood (hemothorax) collecting in the sac around the lungs. It is a very rare complication. If it happens, a drainage will be placed to resolve the air or blood.
- Swelling, bruising or bleeding at the incision site on the chest. Such a complication is rarely severe, and usually occurs the first days after the procedure. It is more common among patients who are on blood-thinning medication.
- Infection at the incision site: Usually occurs the first weeks after the implantation but can also occur later. This is a severe complication that needs immediate treatment.
- Dislocation (movement) of the electrodes: This can occur either during or just after the procedure and will need a repeat operation.
- Infection on the battery or leads: Fortunately rare but a severe complication. Can appear long time after the procedure and need special treatment.
- Even though uncommon, damage to the nerves or blood vessels close to the pacemaker implantation site can occur, leading to local discomfort.
If not stated otherwise by your doctor, you should be able to return to your job and daily activities within a couple of weeks. You do not need to restrict arm movements and/or use an arm sling after device implantation, as this has not been shown to reduce risk of lead dislodgment and may increase shoulder pain. Before resuming your exercises/sports, it is best to consult your doctor for advice. If your stitches need to be removed, your doctor will inform you when and where to do it. Regarding driving, you should ask your doctor for instructions.

